Conditions
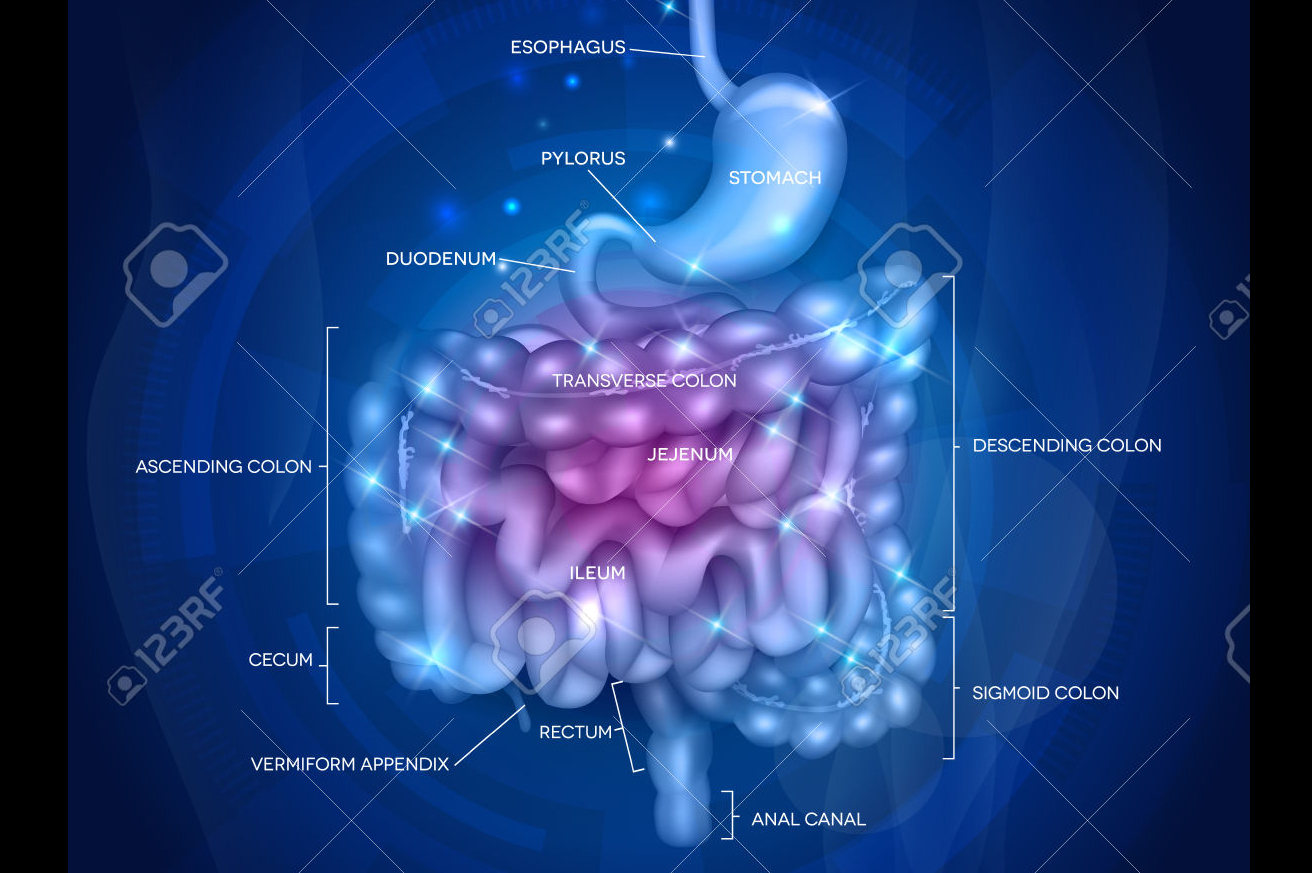
Gastrointestinal Conditions and Disorders
Your body’s digestive system (also called your gastrointestinal system or GI tract) plays a key role in your overall health and well-being. Click on each condition to find out more information.
Barrett’s Esophagus
Barrett’s esophagus is a complication of chronic acid reflux, also known as gastroesophageal reflux disease (GERD).
One change that can occur is called metaplasia: the process of the reversible substitution of a distinct kind of cell with another mature cell of another differentiated kind. This occurs when the body starts growing intestinal cells, rather than esophageal cells, in the esophagus because of the acid influx. If the stimulus that caused the metaplasia is removed, tissues can return to their normal pattern of differentiation. If a metaplasia is not addressed in a timely fashion, it can become dysplasia and/or turn cancerous.
Dysplasia comes from the root Greek term meaning “bad formation.” It is the term used to refer to an irregularity that hinders cell maturation within a particular tissue. Dysplasia is the earliest form of pre-cancerous lesions recognizable in a biopsy, and it is typically referred to as low-grade dysplasia or high-grade dysplasia. Low-grade dysplasia means that the cells show small signs of change, while high-grade dysplasia represents a more advanced condition which may progress to esophageal cancer.
Although the risk of esophageal cancer is small, monitoring of Barrett's esophagus focuses on periodic exams to find precancerous esophagus cells. If precancerous cells are discovered, they can be treated, through procedures such as ablation, to prevent esophageal cancer.
Symptoms of Barrett’s esophagus
- Frequent heartburn
- Difficulty swallowing food
- Chest pain
- Upper abdominal pain
- Dry cough
These symptoms for Barrett’s are similar to acid reflux symptoms; however, many people with Barrett’s have no signs or symptoms.
Risk Factors for Barrett’s esophagus
- Chronic heartburn and acid reflux- having these symptoms of GERD for more than 10 years can increase the risk of Barrett’s esophagus
- Gender- Men are more likely to develop Barrett’s esophagus
- Race- White people have a greater risk of the disease than do people of other races
- Age- Barrett’s esophagus is more common in older adults, but it can occur at any age
Tests to Diagnose Barrett’s esophagus
- Upper endoscopy- can be performed to diagnosis Barrett’s and determine what degree of dysplasia has occurred in your cells. During the procedure, the doctor can examine the esophagus and remove tissue samples for testing.
Treatment for Low-Grade Dysplasia of Barrett’s esophagus
- Maintain a healthy weight
- Eat smaller, more frequent meals
- Avoid tight fitting clothes
- Eliminate heartburn triggers
- Avoid stooping or bending
- Avoid lying down after eating
- Raise the head of your bed
- Quit smoking
Treatment for High-Grade Dysplasia of Barrett’s esophagus
- Surgery to remove the esophagus
- Removing damaged cells with an endoscope
- Using heat to remove abnormal esophageal tissue
- Using cold to destroy abnormal esophagus cells
- Destroying damaged cells by making them sensitive to light
If you undergo treatment, other than surgery to remove your esophagus, there is a chance that Barrett's esophagus can recur. For this reason, your doctor may recommend continuing to take acid-reducing medications and having periodic endoscopy exams.
Liver Disease
Liver disease, also called hepatic disease, refers to a number of diseases that may affect the liver and its function. The liver plays a role in the production of bile, blood-clotting factors and amino acids, and aids in the processing and storage of iron for red blood cell production.
Some of the diseases that affect the liver include infectious hepatitis, cirrhosis (scarring of the liver), liver failure, Gilbert’s syndrome, cancers, bile flow abnormalities and blood flow abnormalities. Some medications may also cause liver damage, including acetaminophen (Tylenol). Treatments for these conditions vary depending on the disease and its causes.
Symptoms of Liver Disease
Because there are so many different types of liver conditions, symptoms will vary. It is imperative that you do not ignore persistent symptoms and allow them to go unchecked.
- Nausea and vomiting
- Abdominal pain in the upper right part of the abdomen
- Swelling of the abdomen
- Dark urine
- Chronic, itchy skin
- Jaundice (yellowing of the skin due to high concentrations of the bile pigment bilirubin).
- Yellowish eyes
- Unexplained fatigue
- Weakness and weight loss
Risk Factors for Liver Disease
Many types of infectious liver disease begin with coming into contact with other people’s bodily fluids. Medical and healthcare professionals are at increased risk for hepatic disease.
- Any profession that exposes you to bodily fluids
- Blood transfusions before 1992
- Body piercings and tattoos
- Heavy alcohol use
- Shared needles from injected drugs
- Diabetes
- Obesity
- High level of triglycerides in the blood
- Unprotected sex
- Working with certain chemicals or toxins
Tests to Diagnose Liver Disease
Because the liver has so many functions, the term “liver disease” is very broad. There are hundreds of types of liver conditions but the most common testing methods to diagnose liver problems include the following.
- Imaging- Computed tomography (CT) scans, x-rays, magnetic resonance imaging (MRI) ultrasound, and magnetic resonance elastography are often used to help diagnose hepatic issues.
- Biopsy- Tissue samples from the liver can indicate disease.
- Blood testing- a simple blood sample can test for liver function, infectious hepatitis or inherited conditions.
- Genetic testing- Members of the same family can be tested for diseases that are genetic in origin.
Treatment for Liver Disease
Liver conditions can sometimes be treated with medications, surgery or even transplant, depending on the condition and severity.
Lifestyle Changes to Treat/Prevent Liver Disease
You can take precautions to prevent liver disease. Although some liver conditions are genetic, there are many conditions that can be prevented.
- Abstain from alcohol or drink in moderation- Women should have no more than one drink per day and men should have no more than two drinks per day.
- Stay current with vaccinations- Talk to your doctor about getting immunized for hepatitis A and B, especially if you are at risk for contracting the hepatitis virus.
- Avoid high-risk behaviors- a high level of risk accompanies the use of illicit drugs, unprotected sex, tattoos and body piercings. Know the risk when you engage in these choices.
- Avoid other people’s blood and body fluid- Hepatitis can be contracted when you come into contact with body fluids or when fluids have not been cleaned properly. Be aware of how hepatitis is spread. You can even contract the virus by sharing a razor or a toothbrush.
- Eat a healthy diet and maintain a healthy weight- Talk to your doctor about what weight is right for you, and use fresh fruits and vegetables and whole grains as the building blocks of your diet.
- Be conscientious about medication- Use medication only when necessary and do not mix alcohol and medication.
Crohn’s Disease
Crohn’s disease is a type of inflammatory bowel disease (IBD). This chronic disorder causes inflammation in the digestive tract, also known as the GI tract, which can lead to abdominal pain, diarrhea, rectal bleeding and other symptoms.
Crohn's disease may be difficult to diagnose because its symptoms are so similar to other intestinal disorders. These symptoms can range from mild to severe and may develop gradually or can come on suddenly. Some people with Crohn’s may experience periods of remission where they have no symptoms.
Warning Signs and Symptoms
- Abdominal pain and cramping
- Diarrhea
- Bleeding from the rectum
- Weight loss
People with severe Crohn’s disease may experience these symptoms as well:
- Fever
- Fatigue
- Joint pain
- Skin disorders
- Mouth sores
- Eye inflammation
- Inflammation of liver or bile ducts
The exact cause of Crohn’s is unknown, but there are a number of factors that can contribute to the development of Crohn’s disease
Risk Factors
- Immune system- It's possible that an infection may trigger Crohn's disease. When your immune system tries to fight off viruses, an abnormal immune response causes the immune system to attack the cells in the digestive tract, too.
- Hereditary- Crohn’s is more common in people who have a family history of the disease.
- Age- While Crohn’s can occur at any age, you are more likely to develop this disease when you are young. Most people develop Crohn’s before they are 30.
- Ethnicity- Whites have the highest risk factor for developing Crohn’s disease, but it can affect any ethnic group. If you’re of Eastern European Jewish decent, your risk is higher.
- Smoking- Cigarette smoking is the most controllable risk factor. It leads to more severe disease and a higher risk of surgery.
- Where you live- People living in urban areas or in an industrialized country are more likely to develop Crohn's disease. Environmental factors, including a diet high in fat or refined foods, play a role in Crohn's disease.
Crohn’s disease can lead to a number of complications such as bowel obstruction, fistulas (abnormal connections between the GI tract and other parts of the body), anal fissures and malnutrition. Crohn’s may also increase your risk for developing colon cancer.
Tests to Diagnose Crohn’s Disease
- Blood tests
- Fecal occult blood test
- Colonoscopy
- Flexible sigmoidoscopy
- CT scan
- Magnetic resonance imaging
- Capsule endoscopy
- Double balloon endoscopy
- Small bowel imaging
- Barium enema
There is currently no cure for Crohn’s disease and there is no one treatment that works for everyone. Medical treatment can reduce the inflammation that triggers the signs and symptoms of Crohn’s and can also limit complications. Medical treatment can also lead to long-term remission as well as symptom relief. The types of drug therapy include anti-inflammatory drugs, immune system suppressors and antibiotics. If diet and lifestyle changes along with drug therapy do not improve symptoms, your GI may recommend surgery to remove the damaged portion of your GI tract.
Colon & Colorectal Cancer
Colon cancer forms in the lining of the colon. Rectal cancer forms in the lining of the rectum, the last several inches of the large intestine terminating in the anus. Either of these cancers is called colorectal cancer.
In the United States, colon cancer is the second deadliest form of cancer when considering both men and women together. Each year about 150,000 people will be diagnosed with colon cancer, and 50,000 people will die from the disease, according to the American Cancer Society.
Though scientists are unsure of exactly what causes colon and colorectal cancer, some risk factors have been identified.
Risk Factors
- Being over age 50
- Polyps, growths inside the colon and rectum that may become cancerous
- A high-fat diet
- Family or personal history of colon cancer or polyps
- Ulcerative colitis, Crohn's Disease or other inflammatory bowel diseases involving the colon
- Sedentary lifestyle
- Diabetes
- Obesity
- Smoking
- Alcohol
- Radiation therapy for cancer
Many cases of colon or colorectal cancer have no symptoms or warning signs until the cancer has advanced. However there are some symptoms that may indicate colon cancer, but these symptoms can sometimes be confused for other conditions such as hemorrhoids. You should consult with your doctor if you experience any of these symptoms and are unsure of the cause.
Warning Signs and Symptoms
- Abdominal pain or tenderness in the lower abdomen
- Bloody stool
- Diarrhea, constipation or other changes in bowel functions
- Narrower than normal stools
- Unexplained anemia
- Unexplained weight loss
- Bloating, fullness or cramps
- Vomiting
Colon Polyps
A colon polyp is a growth of extra tissue in the lining of the rectum or colon. While some can be cancerous, most are not. However, almost all colon cancer does begin as a polyp. Therefore, by removing polyps early, the chances of it growing into colon cancer are eliminated. People with a higher risk for developing polyps are anyone over age 50, those who have had polyps previously or those who have a family history of polyps or colon cancer. However you can still be at risk for polyps or colon cancer without having a family history of either condition. In fact, 80 percent of those who are diagnosed with colon cancer have no family history.
Polyps generally do not cause symptoms. If a patient does have symptoms, they can include blood in their underwear or on toilet paper after a bowel movement, blood in stool, or constipation or diarrhea that has lasted more than a week.
Polyps can be removed during a colonoscopy. If precancerous colon polyps are removed, the chance of the polyp turning into cancer is eliminated. Colon cancer is also highly treatable when discovered early. Depending on an individual's medical and family history, colonoscopies are typically recommended every one, three, five or 10 years.
Treatments and Procedures
The three primary treatment options available for colon cancer are surgery, chemotherapy and radiation. Treatment options for colon cancer depend on the stage of the cancer, whether the cancer has recurred and the patient's general health. The surgical option, a partial colectomy, is the main treatment and includes removing the affected portion of the colon. How much of the colon is removed and whether it is done in conjunction with other treatments will depend on the location of the cancer, how deep it has penetrated the wall of the bowel and if it has spread to the lymph nodes or other parts of the body.
In surgical treatment, the part of the colon that contains the cancer, as well as portions of healthy colon on either side, will be removed to ensure no cancer is left behind. Nearby lymph nodes will be removed and tested at the same time. Usually the doctor is able to reconnect the healthy portions of the colon, but if that is not possible the patient will have a temporary or permanent colostomy bag. A colostomy bag is a device that is worn on the skin discreetly under the clothing and is attached to the remaining bowel. Waste material travels into this bag which is then disposed of, and the bag is replaced as needed. Sometimes, a colostomy is done temporarily to give the bowel time to heal. It may become permanent if too much of the colon or the rectum has to be removed.
If the cancer is small, early stage and localized in a polyp, it is possible it may all be removed during a colonoscopy.
If the cancer is very advanced or the patient's health is extremely poor, surgery may be done simply to provide comfort. This is an operation that will relieve a blockage of the colon to improve symptoms. This will not cure cancer but may relieve pain and bleeding.
Chemotherapy can be used after surgery to destroy any remaining cancer cells, and may be recommended by the doctor if the cancer has spread beyond the lining of the colon. Chemotherapy can be used in conjunction with radiation. Radiation therapy uses powerful energy sources to kill any cancer cells that may remain after surgery or to shrink large tumors before an operation. This option is rarely used in the early stages of colon cancer.
Preventing Colon Cancer
Getting screened is the first step in preventing colon cancer. Several screening options are available, including colonoscopy and flexible sigmoidoscopy. Regular colonoscopies should begin at age 50 for people with an average risk for developing colon cancer. If you have a family history of polyps or colon cancer, many physicians may recommend getting your first colonoscopy at age 40 or even earlier depending on your history. Some recent studies indicate that African-Americans may need to start screening at age 45. More frequent and earlier screening is recommended if you are at high risk for colon cancer.
Lifestyle changes can also be made to reduce the risk of colon cancer:
- Add fruits, whole grains and vegetables to your diet
- Limit saturated fat
- Limit alcohol
- Eat a varied diet
- Quit smoking
- Stay active and maintain a healthy body weight
Gastrointestinal and Gastroenterologist
The term gastrointestinal (GI) refers collectively to the organs of the body that play a part in food digestion. A gastroenterologist is an internal medicine physician who has undergone additional education and training to specialize in gastroenterology, or the treatment of diseases in the gastrointestinal tract and liver.
The term gastrointestinal (GI) refers collectively to the organs of the body that play a part in food digestion. The gastrointestinal tract, also called the digestive tract or GI tract, includes the mouth, esophagus, stomach, small intestine, large intestine (colon), rectum and anus.
Gastroenterologist
A gastroenterologist is an internal medicine physician who has undergone additional education and training to specialize in gastroenterology, or the treatment of diseases in the gastrointestinal tract and liver. Gastroenterologists must complete a three-year residency after medical school, followed by at least one fellowship focused on gastroenterology (fellowships usually last two or three years). After finishing their medical training, gastroenterologists are considered “board eligible” and are qualified to take the Gastroenterology Board Certification test administered by the American Board of Internal Medicine. After passing the exam, a gastroenterologist is “board certified.”
Some gastroenterologists have the letters “F.A.C.P.” or “F.A.C.G.” following their names. These letters mean the gastroenterologist has been recognized as a “fellow” of the American College of Physicians or the American College of Gastroenterologists for making extraordinary contributions to the field of gastroenterology.
Diverticulosis and Diverticulitis
Diverticulosis is a condition when small pouches, called diverticula, form in the wall of the colon. This becomes more common as people get older. About half of people over the age of 60 have diverticulosis. A low-fiber diet can exert more pressure on the colon during bowel movements, which can cause these pouches to form. Diverticulosis does not cause any symptoms until they become inflamed or infected resulting in diverticulitis. These two conditions together are called diverticular disease.
Symptoms of Diverticulitis
- Abdominal pain
- Fever
- Nausea
- Vomiting
- Chills
- Cramping or constipation
Complications from Diverticulitis
- Bleeding
- Colon obstruction
- Abscess
- Fistula (an abnormal connection between the colon and another part of the body)
- Perforation (puncture) through the bowel wall
Tests to Diagnose Diverticulitis
- CT scan
- Barium enema X-ray
- Checking your white blood cells for signs of infection
Because diverticulosis does not cause any symptoms, it is usually identified when a test is being performed for colon cancer screening not for evaluations of digestive symptoms. Diverticulitis may be difficult to diagnose because its symptoms are similar to other intestinal disorders such as irritable bowel syndrome (IBS) and stomach ulcers.
Treatment depends on the severity of your condition. Mild diverticulitis can be treated with rest, changes in your diet and antibiotics. Adding more fiber to your diet can reduce the amount of pressure on your colon and reduce symptoms from diverticular disease. You may also be put on a liquid diet to try and give your colon a rest. Severe cases of diverticulitis may require hospitalization to receive antibiotics intravenously. Occasionally surgery is necessary.
Surgical Treatments for Diverticulitis
- Primary bowel resection- during this procedure your surgeon removes the diseased part of your intestine and then reconnects the healthy segments of your colon
- Bowel resection with colostomy- this surgery may be necessary if you have so much inflammation in your colon that it is not possible to reconnect your colon. During a colostomy, your surgeon makes an opening, called a stoma, in the abdominal wall. The unaffected part of your colon is then connected to the stoma, and waste passes through the opening into a bag.
Hemorrhoids
Hemorrhoids are veins around the anus or lower rectum that have become swollen and inflamed. Hemorrhoids can happen either inside the anus or under the skin around the anus. They are common in both men and women.
Symptoms of Hemorrhoids
- Bright red blood covering the stool, on toilet paper or in the toilet bowl
- Itching
- Pain and discomfort
Both types of hemorrhoids have similar symptoms, but external hemorrhoids may also produce a hard, painful lump that is a result of blood pooling or clotting under the skin.
Treatments for Hemorrhoids
There are a variety of treatment options for hemorrhoids, which may include a warm bath and use of a cream or other medicines. Patients with large hemorrhoids or ones that have not responded to other treatments may need banding or surgery.
Even if you choose to treat hemorrhoids at home, you should see a doctor if there is any rectal bleeding to rule out a more serious condition like colorectal cancer.
Preventing Hemorrhoids
The best way to prevent hemorrhoids is with regular, healthy stools. Stools that can pass easily decrease pressure and straining, which are both risk factors for hemorrhoids. Also, be sure to empty your bowels as soon as possible after the urge occurs.
Lifestyle changes can also help prevent hemorrhoids. Adding exercise to your routine, walking regularly, increasing dietary fiber intake and drinking plenty of water are all ways to help produce soft and easy-to-pass stools.
Helicobacter Pylori (Stomach Infection)
Helicobacter pylori (H. pylori) is a bacterium that causes inflammation of the stomach, chronic gastritis, and ulcers in the stomach or small intestine.
Most people with an H. pylori infection never experience symptoms. When symptoms do occur, it is usually because the bacterium has caused an ulcer to form.
Symptoms of H. pylori
- An ache or burning pain in your abdomen
- Nausea
- Vomiting
- Frequent burping
- Bloating
- Weight loss
This infection is usually acquired in childhood. H. pylori bacteria can be passed from person to person from direct contact with saliva, vomit or fecal matter. It can also be spread through contaminated food and water.
People with H. pylori infections may be more likely to develop cancer in the stomach, including mucosa-associated lymphoid tissue (MALT) lymphoma. The bacterium weakens the protective coating of the stomach and first part of the small intestine, allowing digestive juices to irritate the sensitive lining.
Tests to Diagnose H. pylori
- Blood test
- Breath test
- Stool test
- Upper endoscopy with biopsy
Treatments for H. pylori
H. pylori are usually treated with a combination of two antibiotics. Your doctor will also prescribe an acid suppression drug such as PPIs (proton pump inhibiters) or H2 (histamine-2) blockers to help the lining of your stomach heal. Once the bacteria are completely gone from the body, the chance of its return is low.
Irritable Bowel
Syndrome (IBS)
Irritable Bowel Syndrome (IBS) affects the large intestine (colon) and can cause bloating, abdominal cramping and a change in bowel habits.
IBS is common and more frequently affects women than men. No one knows the exact cause of IBS, but most people can control symptoms with a change in diet, medicine and stress management.
Symptoms of IBS:
- Pain or cramping in the abdominal area
- Diarrhea
- Constipation
- Mucus in the stool
- Flatulence
- Uncomfortable bloating
Risk Factors of IBS
- Being female—more women are diagnosed with IBS than men.
- Family history—People with a close relative, such as a parent or brother or sister, with IBS are at higher risk for IBS. It is unclear as to whether the risk results more from shared genetics or a common environment.
- Being under 35 years of age—At least half of all people who are diagnosed with IBS are under 35 years of age.
Even though IBS is not harmful, it can be confused with other conditions. IBS symptoms may be similar to other diseases such as Crohn’s disease, ulcerative colitis or even colon cancer. It is imperative that you see a doctor if you have significant changes in your bowel habits because IBS symptoms could be an indication of a more serious problem.
Tests to Diagnose IBS
There are no physical signs to diagnose IBS, so diagnosis usually occurs by a process of elimination. To be diagnosed with IBS, the most important symptom is abdominal pain that lasts at least 12 weeks (not necessarily consecutive). Other criteria include mucus in the stool, bloating, bowel straining and urgency and changes in the stool.
If a diagnosis of IBS seems fairly certain, a doctor may recommend treatment without any testing. If there are any reasons for concern, however, a doctor may recommend one or more of the following procedures.
- Colonoscopy- A test that examines the lining of the entire colon to check for polyps, inflammation and abnormalities.
- Flexible sigmoidoscopy- A procedure that uses a flexible tube to examine the the lower part of the colon.
- Computerized tomography (CT) scan- this test will show a cross-section of the internal organs and help diagnose other issues.
- Lactose intolerance tests- if lactase is not present in the body to break down milk sugar, you may exhibit some of the same symptoms as IBS such as cramping, bloating, constipation or diarrhea. This test can help differentiate between lactose intolerance and IBS.
- Blood test- Celiac disease, an allergic reaction to gluten, can have similar symptoms to IBS. A blood test can help exclude celiac disease.
Treatment for IBS
There is no cure for IBS, so the goal is to manage the symptoms.
- Controlling the diet—some people discover that certain foods will trigger IBS symptoms. Common triggers include alcohol, chocolate, carbonated beverages, certain fruits or vegetables or milk. Keeping a food journal and recording foods that cause constipation or diarrhea can be helpful.
- Stress management—like many other diseases and conditions, stress can make IBS worse. Planning ahead, making lists, meditating, taking time to relax and avoiding stressful situations can prevent aggravation of symptoms.
- Fiber supplements—Taking fiber supplements can help control constipation.
- Anti-diarrheal medications
- Anticholinergic medications—these drugs can help control painful intestinal spasms.
Medication for IBS
- Alosetron (Lotronex)—this medication was approved by the FDA, removed from the market, and now is approved again with restrictions. Alosetron helps relax the colon and slow down the bowels. It is only used when diarrhea is the prominent symptoms, and usually used when all other treatments have failed.
- Lubiprostone (Amitiza)—this drug increases fluids in the small intestine to help move the stool. It is generally only prescribed for patients with severe constipation when other treatments have been ineffective.
Peptic Ulcer Disease (PUD)
A peptic ulcer is a sore in the lining of the stomach or first part of the small intestine called the duodenum. When an individual has chronic peptic ulcers, it is known as peptic ulcer disease (PUD).
H. pylori can live in the mucus layer and often causes no problems, but sometimes the bacterium can cause inflammation in the stomach lining and slowly produce an ulcer. H. pylori can be transmitted through food, water, and close human contact.
Another cause of PUD is long-term use of anti-inflammatory medicines like aspirin and ibuprofen. And contrary to popular belief, while stress and spicy foods can aggravate ulcers, they do not cause them. If untreated, peptic ulcers may get worse and cause more serious problems.
Symptoms of PUD
Burning stomach pain is the most common symptom of peptic ulcers and may come and go for a few days or weeks. Pain is more bothersome when the stomach is empty and usually recedes after the patient eats. The burning sensation may become worse at night and is almost always worse on an empty stomach. Sometimes, peptic ulcer disease has more severe symptoms.
- Nausea
- Vomiting of blood—Blood may appear red or black
- Unexplained weight loss
- Loss of appetite
- Dark blood in the stools or tar-like stools
Risk Factors for PUD
- Alcohol—Alcohol can wear away the mucus lining of the stomach and gut, and it also increases the amount of stomach acid that is produced.
- Smoking—Smoking can increase the risk of peptic ulcers for those who are infected with H. pylori.
- Long-term use of pain relievers and/or nonsteroidal anti-inflammatory drugs (NSAIDs).
Tests to Diagnose PUD
- H. pylori test- Doctors can test for the presence of H. pylori in the system by a blood sample, stool sample or a breath test. It can also be diagnosed by obtaining a sample of tissue during endoscopy.
- Endoscopy- an endoscopy is a test that uses a hollow tube with a lens attached. The scope can view the throat, stomach and small intestine and detect an ulcer.
- Biopsy- if an ulcer is found, a small tissue sample will be removed and examined
- X-ray- Swallowing barium (a white liquid) before the x-ray helps doctors see details of the esophagus, stomach, and small intestine as well as view the ulcer
Treatments for PUD
Depending on the cause of the peptic ulcer, treatments will vary.
- Antibiotics—antibiotics can kill the bacterium H. pylori in the digestive system. A two-week treatment should be sufficient, and then antacid medication may be prescribed to control stomach acid.
- Proton pump inhibitors—these medications reduce stomach acid by blocking the action of cells that produce acid. Examples of brand-name proton pump inhibitors are Prilosec, Prevacid, Aciphex, Nexium and Protonix.
- H2 blockers—these medications reduce stomach acid, reduce pain and bring healing. Brand-name products are Zantac, Pepcid, Tagamet, and Axid.
- Antacids—these medications neutralize stomach acid. Side effects can include constipation or diarrhea. Antacids relieve symptoms but do not always produce healing.
If medication does not heal a peptic ulcer, this may be an indication of another issue.
- An infection other than H. pylori
- Zollinger-Ellison syndrome—extreme overproduction of gastric acid
- Stomach cancer
- Crohn’s disease
Lifestyle Changes to Treat PUD
Along with medication, these lifestyle changes may be helpful in assisting to control the pain of peptic ulcer disease.
- Wise diet choices—eating plenty of fresh fruits, vegetables and whole grains may promote healing. Processed foods, fried foods and junk food will make it harder to heal.
- Change your pain reliever—because PUD can be aggravated by using certain pain relievers, talk to your doctor about a different option.
- Stop smoking—Smoking can affect the mucus lining of the stomach and produce more stomach acid.
- Avoid alcohol—Alcohol can wear away the mucus layer of the stomach and intestine.
- Manage stress—Use exercise, mediation, relaxation techniques and recreation to reduce stress and reduce stomach acid production.
Stomach Problems and Swallowing Problems
Most people have experienced some type of stomach problem or discomfort in their lifetime. A person experiencing swallowing problems, which is called dysphagia, may have difficulty swallowing foods or liquids.
Stomach Problems
Most people have experienced some type of stomach problem or discomfort in their lifetime. The stomach stores swallowed food, mixes food with acids for digestion and then transports the mixture to the small intestine. Common stomach ailments include Heartburn, Gastroesophageal Reflux (GER) and Gastroesophageal Reflux Disease (GERD), which occur when food and acids regurgitate and cause discomfort in the throat, chest or upper abdomen. These and other stomach problems may be treated with over-the-counter medications and lifestyle modifications, such as eating healthy, avoiding fatty foods and eating slowly. Other stomach conditions, such as peptic ulcers require medical attention.
Swallowing Problems
A person experiencing swallowing problems, which is called dysphagia, may have difficulty swallowing foods or liquids. Problems swallowing may also cause coughing or choking while eating, slow chewing or eating, gurgling sounds from the throat when eating, hiccups after swallowing and chest tightness or pain after swallowing.
Swallowing problems can happen at any age. Conditions that may cause swallowing problems include nervous system disorders, such as Parkinson’s disease or cerebral palsy; esophageal problems, such as Heartburn, Gastroesophageal Reflux (GER) and Gastroesophageal Reflux Disease (GERD); stroke; head or spinal cord injury; or cancers of the head, neck or esophagus.
Ulcerative Colitis
Ulcerative colitis (UC) is an inflammatory bowel disease (IBD) that causes inflammation in the lining of the rectum and colon. Ulcers form where inflammation has injured the cells that usually line the colon, which then may bleed and create pus.
Ulcerative colitis can be difficult to diagnose because symptoms such as abdominal pain and diarrhea are often seen in other intestinal disorders. About half the people diagnosed with ulcerative colitis have mild symptoms. Others may suffer frequent fever, bloody diarrhea, nausea and severe abdominal cramps. It may also cause problems such as arthritis, inflammation of the eye, liver disease and osteoporosis. It is not known why these problems occur outside the colon, but scientists think it may be the result of inflammation triggered by the immune system. Some of these problems go away when the ulcerative colitis is treated.
Symptoms of UC can also vary depending on the severity of inflammation and where it occurs. Doctors classify ulcerative colitis according to its location.
Classifications of Ulcerative Colitis and Their Symptoms
- Ulcerative proctitis: Inflammation is confined to the area closest to the anus (rectum). For some people rectal bleeding may be the only sign of the disease. Others may have rectal pain and a feeling of urgency (tenesmus). This form tends to be the mildest.
- Proctosigmoiditis: Involves the rectum and the lower end of the colon, known as the sigmoid colon. Bloody diarrhea, abdominal cramps and pain.
- Left-sided colitis: Inflammation extends from the rectum up through the sigmoid and descending colon, which are located in the upper left part of the abdomen. Bloody diarrhea, abdominal cramping and pain on the left side and unintentional weight loss.
- Pancolitis: Affects more than the left colon and often the entire colon. Bloody diarrhea that may be severe, abdominal cramps and pain, fatigue and significant weight loss
- Fulminant colitis: A rare, life-threatening form of colitis affects the entire colon and causes severe pain, profuse diarrhea and, sometimes, dehydration and shock. People with this condition are a risk of serious complications, including colon rupture and toxic megacolon, a condition that causes the colon to rapidly expand.
Causes of Ulcerative Colitis
The cause of ulcerative colitis is unknown. Researchers believed that stress was a possible cause, but they no longer believe that this is a viable explanantion. However, stress can aggravate symptoms. There are now two possibilities for the cause of ulcerative colitis.
- Immune system: some scientists believe that a virus or bacterium may trigger ulcerative colitis. The digestive tract becomes inflamed when the immune system tries to fight off the invading pathogen. It is also possible that inflammation may stem from an autoimmune reaction.
- Hereditary: you’re more likely to develop ulcerative colitis if you have a parent or sibling with this disease. However, most people who have ulcerative colitis do not have a family history of ulcerative colitis.
Risk Factors of Ulcerative Colitis
- Age: While this disease can occur at any age, ulcerative colitis usually begins before the age of 30.
- Race or ethnicity: Although whites have the highest risk of the disease, it can occur in any race.
- Family history: You’re at a higher risk if you have a close relative, such as a parent, sibling or child with the disease.
- Isotretinoin use: Isotretinoin, formerly sold under the brand name Accutane, is a medication sometimes used to treat scarring cystic acne or acne that does not respond to other treatments. While there have been some connections between isotretinoin and ulcerative colitis, the reports are conflicting as to whether isotretinoin actually causes ulcerative colitis.
Complications of Ulcerative Colitis
- Severe bleeding
- Severe dehydration
- Liver disease (rare)
- Inflammation of your skin, joints and eyes
- An increased risk of colon cancer
- A rapidly swelling colon (toxic megacolon)
Tests to Diagnose Ulcerative Colitis
- Blood tests
- Colonoscopy
- Flexible sigmoidoscopy
- Barium enema
- CT scan
Treatments for Ulcerative Colitis
There is no known cure for UC, but therapies are available that may dramatically reduce the signs and symptoms of UC and even bring about a long-term remission. This is either achieved through medications or surgery.
Medications
- Anti-inflammatory drugs
- Sulfasalazine (Azulfidine)
- Mesalamine (Asacol, Lialda)
- Balsalazide (Colazal)
- Olsalazine (Dipentum)
- Corticosteroids
- Immune system suppressors
- Azathioprine (Azasan, Imuran)
- Mercaptopurine (Purinethol)
- Cyclosporine (Gengraf, Neoral, Sandimmune)
- Infliximab (Remicade)
- Adalimumab (Humira)
- Other medications
- Antibiotics
- Anti-diarrheals
- Pain relievers
Surgery
If diet and lifestyle changes, medications or other treatments do not relieve your symptoms, your doctor may recommend surgery. Surgery can often eliminate ulcerative colitis, but that usually means removing your entire colon and rectum.
Lifestyle Changes to Treat Ulcerative Colitis
You can make dietary and lifestyle changes to help alleviate symptoms and lengthen time between flare-ups.
While there is no evidence that says certain foods cause ulcerative colitis, there are certain foods that can aggravate your symptoms. Limiting dairy products and avoiding problem foods may help improve your symptoms. Problems foods can vary for each person, but you should also avoid “gassy” foods such as beans, cabbage and broccoli, raw fruits and fruits, popcorn, caffeine and carbonated beverages. Experiment with fiber. For some, adding more high-fiber foods can help with bowel issues; however, if you have an inflammatory bowel disease fiber may worsen your symptoms. Try eating five or six meals instead of two or three large ones and drink plenty of fluids, preferably water.
Avoiding stress is also a good way to alleviate your symptoms. Stress can aggravate your symptoms, so learning to better manage stress can help. Exercise, biofeedback, regular relaxation and breathing exercises are all ways you can manage stress.
Heartburn, Acid Reflux & GERD
Acid reflux occurs when stomach acid backs up into your esophagus. This may cause heartburn and may ultimately cause damage to the lining of the esophagus. GERD, also known as gastroesophageal reflux disease, is when a person experiences chronic acid reflux.
GERD, also known as gastroesophageal reflux disease, is when a person experiences chronic acid reflux.
Symptoms of Acid Reflux/GE
- A burning sensation in your chest (heartburn), sometimes spreading to the throat, along with a sour taste in your mouth
- Chest pain
- Difficulty swallowing (dysphagia)
- Dry cough
- Hoarseness or sore throat
- Regurgitation of food or sour liquid (acid reflux)
- Sensation of a lump in the throat
Risk Factors of Acid Reflux/GERD
- Obesity
- Hiatal hernia
- Pregnancy
- Smoking
- Asthma
- Diabetes
- Overeating
- Connective tissue disorders, such as scleroderma
People who have GERD or experience acid reflux on a regular basis are at an increased risk of Barrett’s esophagus and esophageal cancer. GERD can lead to precancerous changes in the esophagus, known as Barrett’s esophagus. These changes are associated with an increased risk of esophageal cancer. The risk of cancer is low, but your doctor will likely recommend regular endoscopy exams to look for early warning signs of esophageal cancer.
Tests to Diagnose Acid Reflux/GERD
When acid reflux becomes chronic, there are some procedures and tests that your doctor can perform to diagnose GERD.
- Barium esophagram- an X-ray of your upper digestive system. This procedure requires you to drink a chalky liquid that coats and fills the inside lining of your digestive tract. This allows the doctor to see the shape and condition of your esophagus, stomach and upper intestine.
- Upper endoscopy- by passing a flexible tube down your throat, an endoscopy allows the doctor to visually examine the inside of your esophagus. You doctor might also use the endoscopy to collect a sample of tissue from your esophagus for further testing. This is usually done with sedation.
- Esophageal pH (acid) test- this test monitors the amount of acid in your esophagus. The device used to measure acid can identify when and for how long stomach acid regurgitates into your esophagus.
- Esophageal motility test- this test measures the movement and pressure in your esophagus.
Lifestyle Changes to Treat Acid Reflux/GERD
- Maintain a healthy weight
- Avoid tight-fitting clothes
- Avoid foods and drinks that trigger heartburn (common triggers are fatty or fried foods, tomato sauce, alcohol, mint, garlic, onion and caffeine)
- Eat smaller meals
- Watch portion sizes- larger and higher-fat meals tend to stay in the stomach longer before moving to the small intestine, so the LES and esophagus are potentially exposed to stomach contents/acid for a longer time
- Keep a heartburn/food journal- record symptoms, the time they occurred, what you ate, and activities you engaged in before the discomfort started
- Don’t lie down after a meal
- Elevate the head of you bed
- Don’t smoke
While some people experience acid reflux/GERD and heartburn relief by making changes to their lifestyle or by taking over-the-counter medications such as antacids, H2 blockers and PPIs, others may continue to experience these symptoms. If 4 to 8 weeks of twice-daily PPI therapy is unsuccessful, further investigation with endoscopy is recommended. There are some procedures that can be done to treat GERD.
Treatments for Acid Reflux/GERD
- Nissen fundoplication- surgery to reinforce the lower esophageal sphincter
- Surgery to create a barrier preventing the backup of stomach acid
- Stretta procedure- a procedure to produce scar tissue in the esophagus
- Linx- surgery to strengthen the lower esophageal sphincter
Esophagitis and Stricture
Esophagitis is a general term for any inflammation, irritation or swelling of the esophagus, which is the tube that leads from the back of the mouth to the stomach.
Benign esophageal stricture is a narrowing of the esophagus that can cause swallowing difficulties. It can be caused by gastroesophageal reflux (GER), certain medications, long-term use of a nasogastric tube that runs from the nose to the stomach, swallowing corrosive substances or a bacterial or viral infection. Symptoms can include difficult or painful swallowing, unintentional weight loss or food regurgitation.
info@camarilloendoscopycenter.com
CALL
Phone: 805.275.0200
Fax: 805.275.0211
FIND US
4005 Mission Oaks Blvd. Unit B
Camarillo, CA
OPEN
Monday - Friday
8am – 5:00pm
©2017 camarillo endoscopy center